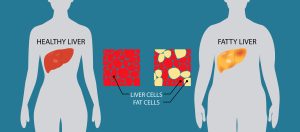
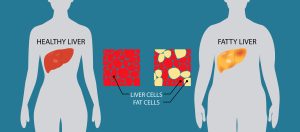
 Steatotic liver disease (SLD), formerly known as fatty liver disease, describes the buildup of excess fat in the liver. A healthy, high-functioning liver contains a small amount of fat. However, fat buildup can become a problem when it reaches over 5% of your liver’s weight.
Steatotic liver disease (SLD), formerly known as fatty liver disease, describes the buildup of excess fat in the liver. A healthy, high-functioning liver contains a small amount of fat. However, fat buildup can become a problem when it reaches over 5% of your liver’s weight.
Healthcare providers classify SLD based on its causes and the conditions associated with it. The types of steatotic liver disease include:
- Alcohol-related liver disease
- Metabolic dysfunction-associated steatotic liver disease (MASLD). Risk factors associated with MASLD include:
- Obesity
- Type 2 diabetes
- High blood pressure
- Lipid normalities
- Metabolically associated steatohepatitis (MASH)
- MASLD and increased alcohol intake (MetALD)
In most cases, the fat buildup in the liver doesn’t cause serious problems or prevent it from functioning normally. In some cases, the condition progresses to liver disease. It usually progresses in stages:
Hepatitis– in this first stage, called steatohepatitis, your liver goes from fatty to inflamed, damaging the tissue.
Fibrosis– in this second stage, causes bands of scar tissue to form where the inflammation damages the liver, causing it to stiffen.
Cirrhosis– in this third stage, extensive scar tissue caused by inflammation replaces healthy tissue. This is called cirrhosis of the liver. Without treatment, cirrhosis can lead to potentially fatal conditions like liver failure and liver cancer. About 90% of people who develop hepatocellular carcinoma (a type of liver cancer) have cirrhosis.
Steatotic liver disease doesn’t always cause symptoms. When they are present, symptoms can include:
- Abdominal pain or a feeling of fullness in the upper right side of your abdomen
- Extreme exhaustion or fatigue
People will more commonly notice symptoms once SLD has progressed to cirrhosis of the liver. When cirrhosis develops, you may experience:
- Nausea
- Loss of appetite
- Unexplained weight loss
- Jaundice
- Swelling in the abdomen
- Swelling in the legs, feet, or hands
- Bleeding in the esophagus, stomach, or rectum
Steatotic liver disease has multiple causes. You are more likely to develop SLD if you have a cardiometabolic risk factor, if you consume unhealthy amounts of alcohol, or both. You have a greater chance of developing SLD if you have the following:
- Alcohol use disorder
- Metabolic syndrome
- Type 2 diabetes
- Are overweight (a BMI of 25 to 29.9 kg/m2)
- Obesity (a BMI of 30 kg/m2 and above)
- Polycystic ovary syndrome (PCOS)
- Obstructive sleep apnea
- Hypothyroidism
- Hypopituitarism
- Hypogonadism
- Take certain prescription medications
Without treatment, a steatotic liver can progress to cirrhosis of the liver, which can lead to liver failure, liver cancer, and cancers outside the liver. People with MASLD are also at increased risk of heart disease, which is the leading cause of death in people with MASLD.
Because SLD doesn’t usually cause symptoms, a healthcare provider may be the first person to notice an issue. High levels of liver enzymes that turn up on a blood test for other conditions can raise a red flag. Elevated liver enzymes are a sign of liver damage.
To diagnose SLD, a healthcare provider may ask about your medical history and perform a physical exam, imaging tests, and a liver biopsy.
There are no specific treatments or medications for SLD. Instead, healthcare providers focus on helping you manage risk factors that contribute to the condition. This can include making lifestyle changes that can improve your health. Your healthcare provider may recommend that you:
- Avoid alcohol
- Lose weight
- Take medications to manage metabolic conditions
- Get vaccinated for hepatitis A and hepatitis B
A healthcare provider may change your prescriptions if your medicine is causing fat to accumulate in your liver.
The best way to avoid SLD is to maintain your overall health. You can prevent SLD by:
- Exercising regularly
- Limiting your alcohol consumption
- Maintaining a weight that is healthy for you
- Taking medications as prescribed if you have Type 2 diabetes or metabolic syndrome.
Working with a specialist at Flushing Hospital Medical Center’s Ambulatory Care Center can help you determine your biggest risk factors for liver damage, identify medications that may lead to further damage, and find the right treatment for any scarring or disease you are experiencing. To schedule an appointment, please call (718) 670-5486.
All content of this newsletter is intended for general information purposes only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.
 April 26th, 2025, is observed as the Drug Enforcement Administration (DEA) National Prescription Drug Take Back Day. It is a day that encourages the public to remove unneeded medications from their homes as a measure of preventing misuse and opioid addiction from ever starting.
April 26th, 2025, is observed as the Drug Enforcement Administration (DEA) National Prescription Drug Take Back Day. It is a day that encourages the public to remove unneeded medications from their homes as a measure of preventing misuse and opioid addiction from ever starting.